Dr. Stec’s Heartworm Schpeel
Arkansas is currently #3 in the nation for heartworm cases
I like to tell my clients “Parasites love Arkansas.” It’s true, and, as veterinarians, we see a lot of parasites on a daily basis. So much so that we spent two semester classes devoted solely to parasites when I went to vet school. Heartworms are one of the major parasites we study. As mosquito populations are changing, heartworms are becoming increasingly more common in the Arkansas River Valley. According to the American Heartworm Society, Arkansas is currently #3 in the nation for heartworm cases.
What is it?
What it sounds like – literally worms in your dog’s heart. This leads to lung and cardiac damage as well as heart failure. The scientific name of the most common heartworm is Dirofilaria immitis. The microfilaria (babies) are carried by mosquitoes. Mosquitoes feed on a pet and inject the microfilaria. Those microfilariae develop into several different stages of larva. The larvae then grow into adult heartworms in dogs’ left ventricle and pulmonary artery (main vessel that goes from the heart to the lungs.) If there are both sexes of heartworms, they then reproduce and microfilaria are released into the bloodstream. Mosquitos feed and the cycle continues. The heartworm life cycle is about seven months long, but adults often live for 5-7 years if the pet does not succumb to the parasite.
Who gets it?
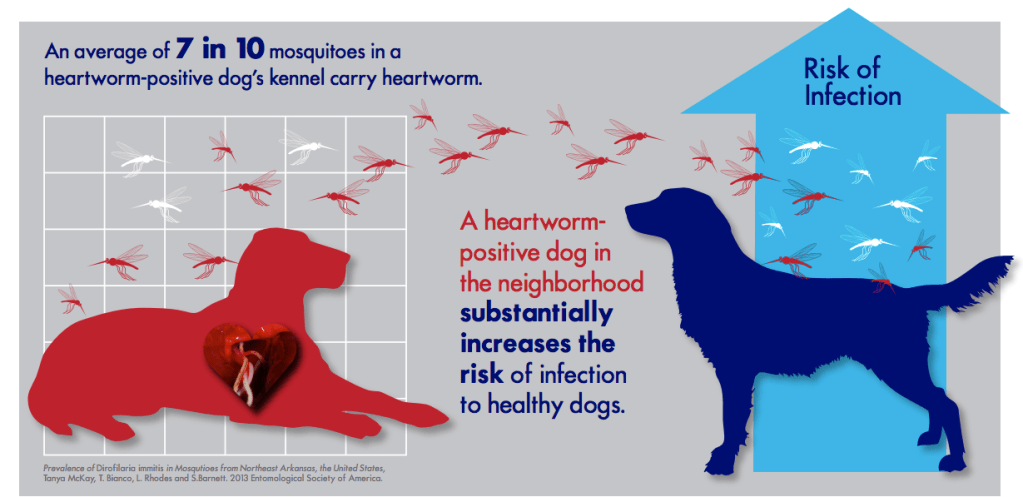
Lions, tigers, and bears, oh my! Dogs are the primary natural host for heartworms and all dogs in endemic areas are susceptible (even indoor dogs who just go outside to potty). IT IS RECOMMENDED THAT ALL DOGS IN THE ARKANSAS RIVER VALLEY STAY ON A HEARTWORM PREVENTATIVE. Cats can contract heartworms, but they are not the standard host for the parasite. In cats, only one or two adults develop and then cause lung inflammation. Coyotes, ferrets, sea lions, seals, lions, tigers, and bears can also contract heartworm disease. There are few incidents of a human contracting an adult heartworm as an unusual host, but, realistically, humans do not get heartworms.
How are heartworms diagnosed?
Our primary test for heartworms is an in-house heartworm antigen test. The antigen tests for female adult heartworms. False negatives can occur if there is a male only population of adults (uncommon) or if there are immature stages. If a pet has not been on heartworm preventative or has had a lapse in their preventative schedule (which happens to the best of us), a recheck test should be performed six to seven months after an initial negative test to fully confirm negative status. Your veterinarian may also do a microfilaria check – a simple evaluation of the blood under the microscope to look for the microfilaria. There are also changes on chest radiographs that can lead to a heartworm diagnosis. Dogs with heartworm disease may have clinical signs of coughing, exercise intolerance, lethargy, and / or weight loss. In advanced cases, dogs will develop a swollen abdomen.
What kind of preventative do I use?
There is a plethora of preventatives available. Monthly preventatives generally combine an intestinal dewormer and perhaps a flea control. There are also six month and twelve month injections available. Your veterinary clinic can help you choose which preventative is best for your pet’s lifestyle. The most important part is that they stay on something. Heartworm preventative is a PRESCRIPTION. If you are getting it online without your veterinarian’s approval, it’s likely a counterfeit. If you are getting it from the pet store, you’re likely just buying a flea and/or tick control. There is no effective “natural” or home remedy type preventative. However, preventatives are not synthetic compounds.
Why is it a prescription?
Preventatives are rather safe. However, if a heartworm positive dog is given a preventative there is an increased risk of an embolism. Preventatives are part of the treatment for positive dogs, but are given under veterinary guidelines with additional medications. Also, your veterinarian may choose specific preventatives for dogs with seizure disorders.
If a dog has heartworms, can it be treated?
Most of the time, yes. Treatment is somewhat complicated but involves several injections of a drug called immiticide. A positive dog will require cage rest for several months during treatment. “Slow kill” is available in certain scenarios, but is not recommended by the American Heartworm Society. Slow kill takes approximately two years. It is discouraged due to the potentiation of heartworm resistance and that the worms will still be doing damage during the long treatment. Dogs will also be at risk of embolism during those two years. In advanced cases, surgical removal by a specialist may be necessary. Unfortunately, cats cannot go through immiticide treatment.
Where can I find more information?
Visit heartwormsociety.org for a wealth of heartworm information. As always, your veterinary staff can answer most questions regarding the disease.
If you need a test, come see me at Alma Animal Clinic! Or, you may find me serving as a relief veterinarian at a local clinic. Give your furry kiddo hugs from me!
-Nicole Stec Phillips, DVM

References
Heartworm Basics. (2020, February 20). Retrieved from American Heartworm Society: https://www.heartwormsociety.org/pet-owner-resources/heartworm-basics